
Care of the Virginia Opossum

Copyright 2005 © Laura Mowrey - All Rights Reserved
No one may copy or reproduce the contents of this website without written permission of the owner.
This page is dedicated to the anatomy and misc medical issues of the Virginia Opossum
Basic Anatomy:
The purpose of these pages is to show miscellaneous pictures of opossum anatomy as well as some their medical issues.

The penis of the male opossum is "bifurcated" or split on the end. This trait is true of all marsupials. It is interesting to note that on opossums, the testicles are located "in front of" the penis, rather than behind it.

Here we have an example of a hermaphrodite: in this case, an opossum having both male and female sex organs or other sexual characteristics. This opossum has both a penis and a pouch.

Anatomy of a female's reproduction organs. Note how the vaginal regions split off to both the left and the right, thus the need for the male’s penis to be split on the end.
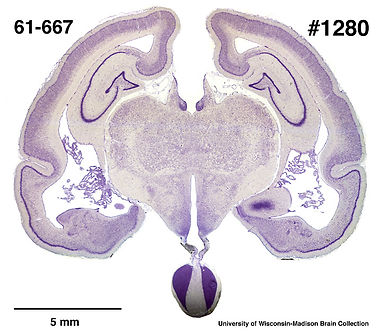
Coronal section through middle of brain.

Whole brain photographs.

Opossum Skull.
Medical Issues:
Below are some various medical issues that can occur in opossums, but by no means is this a complete picture. Please refer to other pages on this site for more complete information.


Here is an example of an obese female opossum. Note the size of her tail (especially at the base) and the fat deposits in the outside corner of her eyes. This female was not over-fed and her owner followed the NOS diet guidelines. She also had free run of a very large home. Might it be possible for some opossums to be predisposed to obesity like some humans are?

You can purchase special carts for opossums that need assistance walking, from most manufacturers who make these carts for dogs and cats. You can also go onto YouTube and search "how to make a dog wheelchair."


In this first photo you can see where Kizzie's bladder bulged from his body. As he grew older, his spinal deformity advanced, causing his bladder to protrude. The 2nd photo shows you just how injured his spinal column was, as well as his tail, which was broken at the base. This picture was taken when Kizzie was 3 years old. Taking these photos during his bath made his condition much more visible. Despite this babies rough start in life, he lived to be 4 1/2!

Photos Compliments of: Mary Strait

Full Anal Glands:
Notice the swelling on both sides.
Anal glands after they have been expressed;
This is the liquid that came out of them.
Treatment consists of any one or all of the following:
-
Sometimes soaking the animal is warm water will loosen them up enough so that they can be gently expressed.
-
Other times more aggressive measures must be taken, where they lance the area, remove the impacted material and allow to further drain.
-
Antibiotics are always indicated, in the later 2 scenarios.
Adding fiber to the diet can sometimes help prevent this from re-occuring, as can frequent evacuations. If these measures fail, sometimes the anal glands have to be removed altogether. Great care must be taken to express the anal glands on any animal so as not to dmage the area or cause undue pain.



Preparing to clear the anal glands
There is a over the counter medication I found online that is supposed to help animals with anal gland issues. It's called "ANAL GLANDZ" and is sold by a company called PetAlive online. I have never used this product so use this at your own discretion:
http://www.nativeremedies.com/petalive/products/analglandz-support-cat-dog-anal-glands.html


Buck shot :(
X-ray of a female, look at the babies this female is carrying in her pouch!


Spinal deformity

A different view of her spine.
Case Studies:
These are before and after pictures of an abcess Connie found on one of her possums. She squeezed out all of the bacteria, cleaned the area well, placed sugar inside the opening and is treating him for 14 days with dicloxicillin for 14 days to knock out the infection. As you can see, its clearing up really well.




Photos and Information Compliments Of:
Connie Welborn Reese
Cellulitis:
As told to me by Arina Hinzen:
"After all other tests came back negative (mange, fungal, bacterial) and because it was so spread out over her body, my vet as very sure that we were dealing with "juvenile cellulitis". It appears that it originally started around her nose and eyes. I had her on a high dosage of Amoxicillin and injectable Baytril and of course Nystatin. I would have rather had her on Dicloxacillin but the meds came in so late and she had already started to respond so well to the other antibiotics. In addition I used topical a mix of dilluted therapeutic grade essential oils which seemed to have a very soothing effect on her skin. And of course fluids, fluids, fluids the first two days. I'm still nervous that what ever it as might come back and keep a very close eye on the little girl. Right now, she's looking really good!"
Before: Note the discolored fur and swollen eyes and paws:


After: Look at the huge difference since treatment began
(Baby on the far right):

Photos Compliments Of: Arina Hinzen
Case study: Infected Tail:
Submitted By; Sally Robertson


Appx date lesion was noticed: October 30th
It first appeared as a sort of raised area that was normal in color (skin toned). Later it took on a sort of dark brownish reddened area, and this substance had a bad odor and was gooey and waxy.
Vet Appt: Nov 2nd
The Vet took a scraping to be sent out for cytology and histology screenings. The initial report from the cytology on Allie's wound showed it is a glandular cystic rupture, with a secondary inflammatory reaction.
Microscopic Description: Idexx Laboratories
The smear is of good quality and consists of many large clusters of superficial squamous epithelial cells with a background of bluish amorphous material and a few fragments of hair shafts. There is moderate to severe infiltration of well-preserved neutrophils with smaller numbers of eosinophils, macrophages, and occasional mast cells. There are free mast cell granules in the background. There is no evidence of sepsis or cells showing prominent criteria for malignancy.
Cytology Interpretation:
An epidermal inclusion/follicular cyst with secondary mixed inflammation is the primary consideration.
Comments:
The inflammation is most likely secondary to rupture of the lesion and leakage of keratin in surrounding tissues (acts as foreign material). A small foreign body could also create a similar inflammatory response and the squamous epithelial cells could be in larger numbers due to the scraping method to obtain the sample.
The report came back as positive for:
-
E-coli
-
Enterococcus
Condition was reported to be sensitive to the following medications:
Cefotaxime
Ceftazidme
Ceftiofur
Imipenem
Amikacin
Gentimicin
Tobramycin
Ciprofloxacin
Enrofloxacin
Tetracycline
Chloramphenicol
Trimethoprim-Sulpha
For amoxicillin susceptible isolates, treatment with amoxicillin, ampicillin or penicillin is recommended. Other antibiotics to which the isolate is susceptible should be considered as secondary options reserved for the treatment of amoxicillin-resistant isolates.
Topical Treatments Used: (In order of usage)
-
Sugar
-
Neosporin
-
Chlorexidrine (to cleanse the area with)
-
Manuka honey
-
Vinegar
-
MicroTek shampoo
-
Silver sulfadiazine gel
-
Veteriycin VF (to cleanse the area with)
-
Vitamin A
-
Vetricyn VF spray
Oral antibiotic treatments:
-
1 week Clavamox
-
4 weeks Orbax (ending Dec 20, 2015)
Despite all of the above treatments, to date, Dec 18, 2015, the lesion has increased in size and has a bad odor emanating from it. When scraped, we are still getting a gooey sort of waxy substance off of it.
She has a history of DSN as a small baby when she first arrived here, that appeared to clear up after several weeks of amoxicillin. The only lesions she had were on her ears.
She has always been a excellent, voracious eater, but her appetite has been up and down this past month or so. She has been fairly active, running on her wheel, interspersed with a few nights where she didn't appear to get out of her bed at all.
Next step will be another Vet visit with a request for blood work.




These images were taken in December. As you can see, the area is larger, more raised and is showing no improvement.
March; While all signs of infection are gone, This female still has a raised area that we have to keep scrupulously clean to prevent re-infection. We are looking at laser treatments to get rid of it completely.
Listeriosis:
Listeriosis:
Listeriosis is a disease of the central nervous system and a infection can occur when an animal ingests anything that has been contaminated with bacteria called Listeria monocytogenes (L. monocytogenes). Listeriosis is probably severely under diagnosed in our opossums for obvious reasons. This bacterium can live almost anywhere--in soil, manure piles, and grass. Animals infected with Listeria can show signs restlessness, loss of appetite, fever and nervous system disorders. Although not seen in every case, the most notable symptom gives this disease its nickname, "Circling Disease." Other, more subtle symptoms include uncoordinated movements, leaning against objects, and progressive paralysis. Death can occur within 2 to 3 days after the onset of symptoms. Healthy animals are not usually affected by Listeria. Recognition of symptoms is important for successful treatment. Most animals will recover if treated with a broad spectrum antibiotic started early.
Causes:
The bacterium Listeria monocytogenes is found in wild animals, domesticated animals, and in soil and water. These bacteria make many animals sick, leading to miscarriage and stillbirth in domestic animals.
***Vegetables, meats, and other foods eaten can get infected with the bacteria if they come in contact with contaminated soil or manure. Raw milk or products made from raw milk may also carry these bacteria.
Symptoms:
-
Loss of appetite
-
Circling, uncoordinated movements, leaning and progressive paralysis
-
Lethargy
-
Jaundice
-
Respiratory distress (usually pneumonia)
-
Shock
-
Skin rash
-
Vomiting
-
Abscesses
-
Conjunctivitis
-
Gastroenteritis
-
Skin lesion(s)
Listeriosis in babies results in a poor outcome with a high death rate. Healthy older animals have a lower death rate. Babies who survive listeriosis may have long-term brain and nervous system (neurological) damage and delayed development.
Head Trauma:
Signs of head trauma include one or more of the following:
-
Circling/Abnormal gait
-
Crackling noises coming from the sinuses
-
Nasal bleeding
-
Ear canal bleeding
-
Dislocated/fractured jaw
-
Pupils narrowed and or unresponsive to light
Treatment:
The treatment for head trauma depends on the severity of the animals condition. It is ALWAYS advisable to get the animal to a qualified and knowledgeable Vet. At the very least, medication for pain and hydration procedures should be done. I always use a homeopathic medicine called Arnica Montana with ANY injury as it helps with inflammation and swelling. Keep the animal in a quiet room with subdued lighting.
SPUDS: (Sudden Possum Unexplained Death Syndrome:
Infants can easily contract infections through the dead mother's milk or from breathing in an infectious organism. In addition it can also be caused from the use of unsterilized feeding implements or unwashed hands. It can also be caused if bowel stasis has occurred, as it often does in cases of shock, trauma or hypothermia. In systemic infections amoxicillin is the antibiotic of choice. DO NOT WAIT for symptoms of illness to occur in your babies before you treat with amoxicillin because by the time you are seeing symptoms, it can be too late to turn them around. All incoming babies should be placed on amoxicillin and nystatin whether they appear ill or not. Nystatin is an antifungal and it is needed to combat overgrowth of yeast in the oral cavity and GI tract from the use of antibiotics.